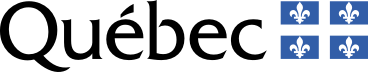
Between 70 and 80% of sexually active women will become infected with human papillomavirus or HPV—one of the most common viruses in the world. In some, HPV will cause precancerous lesions. Every year in Québec, 53,000 women consult a specialist for further testing after receiving the abnormal results of a screening test carried out during a routine gynecological examination.
Only those who test positive should then undergo a colposcopy and biopsy.
In the case of a pre-cancer diagnosis, they may undergo minor surgery to remove the problematic cells before they become cancerous. In the two years after the procedure, patients have follow-up colposcopies of their cervix and biopsies. But 90% may not need such close monitoring, affirms Dr. Marie-Hélène Mayrand, professor in the departments of Obstetrics and Gynecology and Social and Preventive Medicine at Université de Montréal and researcher at the Centre de recherche du CHUM. Is it possible to prevent cervical cancer and avoid unnecessary interventions?
To answer the question, the gynecologist and epidemiologist compared various follow-up methods in nearly 2,000 Canadian women treated for cervical pre-cancer. The study mobilized 13 research teams across the country that worked to determine the best strategy to identify failed surgeries, which occur in 10% of patients operated. The early findings indicate that, six months after the intervention, HPV testing should be carried out in all the women to determine whether their cervical cells still carry the virus.
Only those who test positive should then undergo a colposcopy and biopsy. The others would only require a follow-up with their family physician and a Pap test to detect cervical cell anomalies. Dr. Mayrand hopes that these results will improve the efficiency of cervical cancer screening programs and reduce the costs by dedicating resources to the highest risk patients.